Venous Ulcer of Lower Leg
History:

Fig.1. Ulcer at first visit.
Findings:
Diagnosis:
Differential Diagnoses:
Workup Required:
Plan:
Expertise Needed:
Treatment:
Using local anesthesia as needed, adherent devitalized tissue was debrided using scalpel and hydro jet. The borders of ulcer with thickened, raised edges was excised. No punch biopsy to rule out malignancy was necessary. Biofilm was removed with hydro jet during debridement. An antimicrobial agent (hypochlorus acid) was then applied together with an interface dressing plus a moist foam dressing. A short stretch compression bandage was applied from the foot to the knee. The patient was scheduled for outpatient skin grafting one week later and for another debridement in between.
One week later, the ulcer was again debrided and then micro grafted under local anesthesia as outpatient surgery. A split thickness skin graft of 25 cm square was harvested with a hand held dermatome (Xpansion, DSN, Charlestown, NH). It was then minced with a hand held mincer (Xpansion, DSN, Charlestown, NH). The minced skin particles were then spread uniformly over the wound with a spatula. The grafted area was covered with an interface dressing (Tegaderm Contact, 3M, St Paul, MN.) On top of this was placed a thin layer of hydrogel and then a “moist” foam dressing. A short stretch compression bandage was then applied. The patient was advised to keep the leg elevated.
Three, seven and ten days after surgery the patient returned for dressing changes. The hydrogel, Foam and compression bandage were replaced but the interface dressing was left in place. On postoperative day 14 and then weekly, the interface dressing was also replaced.

Fig.2. Ulcer with micro grafts before application of hydrogel and dressing.
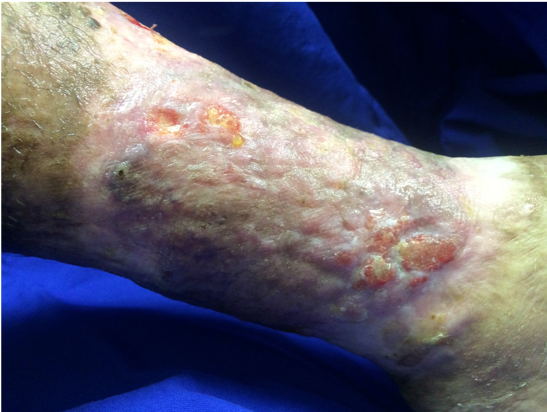
Fig.3. Grafted ulcer 3 weeks postoperatively.

Fig.4. 8 weeks after grafting, the ulcer is almost completely healed.
Follow Up:
Three weeks after grafting, the ulcer was mainly healed. Dressing changes were then done every 2 weeks and at 8 weeks the ulcer was almost completely healed. It has remained healed for over 2 years. The patient wears a compression bandage every day.

Fig.5. 2 years after grafting, the ulcer remains healed with durable skin quality.

