Subluxation of small finger MCP joint with open wound
History:
53-year-old lawyer who sustained left small finger fracture subluxation with resulting open palmar wound. She was riding a bicycle earlier in the day when she was sideswiped by a car and fell on the side of the street. She suffered some superficial abrasions to her thighs but no other significant injuries. She is left-handed, a non-smoker and had no prior hand trauma. She works mostly from a computer desk and uses her hands to type a lot. She meets with clients via zoom or in person as needed. TDAP-vaccine and Ancef antibiotics were given in the ED. The Plastics and Reconstructive Surgery team was consulted for the small finger injury.
Findings:
Left small finger subluxation at the meta-carpo-phalangeal joint with ulnar deviation. Open wound to radial aspect distal palmar crease of the small finger with bone exposed. Punctate wound to the distal tip. Tendons were intact as were ligaments and the finger had full sensation.





Figure 1 and 2. Shows left small finger injury. Figure 3-5 show initial XRays of left hand.
Diagnosis:
Left small finger meta-carpo-phalangeal subluxation and open wound.
Differential Diagnoses:
None.
Workup Required:
X-rays of the left hand to evaluate for fractures and possible retained foreign bodies.
Plan:
Reduction of subluxated left small finger metacarpal phalangeal joint and repair of laceration under local anesthesia in the Emergency Department.
Expertise Needed:
Plastic surgeon or Hand surgeon.
Treatment:
Local anesthesia with 1% plain lidocaine provided a digital block. The hand was prepped with betadine and draped using sterile towels. The wound was copiously irrigated with normal saline and betadine. Figure 1 shows the left small finger injury. The subluxated joint was first reduced to its anatomical position. With the finger held in place, the laceration was then repaired with interrupted 4-0 Chromic sutures. The hand was then immobilized with placement into an ulnar gutter splint. Repeat X-ray films were obtained confirming the anatomical alignment following reduction.

Figure 3. Shows left small finger after reduction and laceration repair.
Follow Up:
Arm elevation was encouraged to minimize pain and swelling. Tylenol and ibuprofen were used to control pain. Showers were allowed, but no submerging or soaking in water for two weeks. No lifting of over 10 lbs for two weeks. She was first seen for follow up after 1 week. at that time the finger was well reduced and there were no signs of infection. When she was seen for her 1 month follow up, there was no pain in the left small finger and the wound was healed. She had full range of motion of the finger and was able to use the hand without limitations.



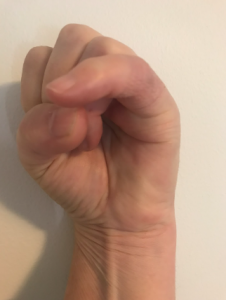
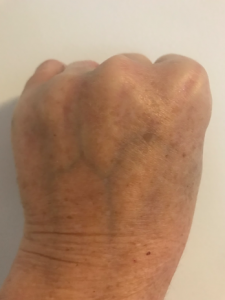
Figure 4. One month follow up.

