Pediatric Subungual Hematoma and Nail Bed Laceration
History:
8-year-old right-handed female patient presenting with right ring finger injury after door slammed shut on finger two days ago. Given worsening swelling and pain, mother decided to present to ED for further evaluation.
Findings:
Significant subungual hematoma limited to dorsal aspect of right RF distal phalanx. Digit otherwise warm and well-perfused, vascularly intact with capillary refill <3 seconds in all finger tips. Palpable radial and ulnar pulse. Flexion/extension intact in wrist. Flexion of FDP/FDS and extension intact in all fingers. Median/radial and ulnar motor function grossly intact with “OK” sign, thumbs up and finger adduction/abduction. Sensation intact in radial, median and ulnar distribution.

Figure 1: Anterior view of the subungual hematoma of right RF.
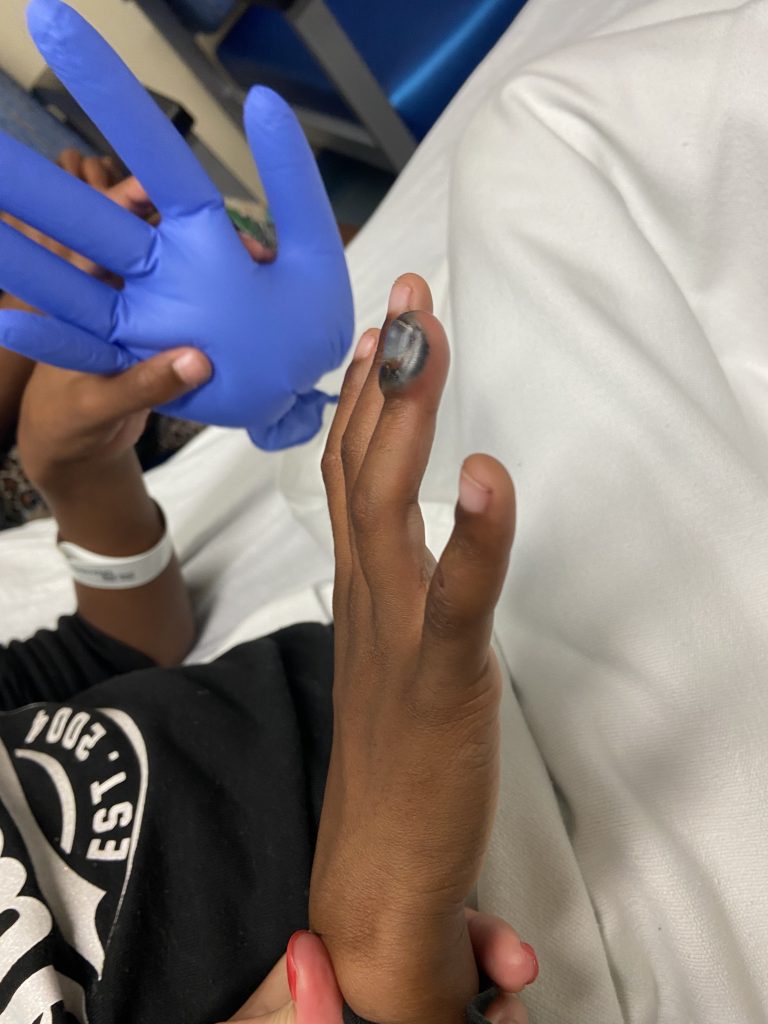
Figure 2: Lateral view of subungual hematoma limited to dorsal aspect of right RF distal phalanx.
Diagnosis:
Right ring finger subungual hematoma with likely nail bed laceration (especially given hematoma >50% of nail).
Differential Diagnoses:
R/O Seymour fracture (displaced distal phalanx physeal fracture with associated nail bed laceration)
Workup Required:
Complete hand exam (as detailed above). Hand and isolated finger XR to rule out Seymour fracture. Xray ruled out Seymour fracture.

Figure 3: Dedicated right RF finger X-ray (lateral view) without Seymour fracture.
Plan:
Wash out, nail removal, nail bed laceration repair in ED.
Expertise Needed:
Plastic or Hand surgeon.
Treatment:
Intra-nasal versed and digital block using 6cc of 1% lidocaine without epinephrine. Nail was removed using a periosteal elevator with immediate drainage of 10cc of blood. Visible nail bed laceration distal to the nail fold. No instability noted of the distal phalanx. Wound thoroughly irrigated with 250cc NS mixed with betadine. Nail bed lac repaired with 5-0 fast gut. Stented nail with original nail which was secured with dermabond. Dressed with bacitracin, xeroform gauze, and kling wrap. Alumafoam splint was applied to prevent accidental trauma to the fingertip and for patient comfort. Patient tolerated the procedure well.

Figure 4: Visible nail bed laceration distal to the nail fold.

Figure 5: S/p nail removal and nail bed repair.
Discharge Instructions:
- Keflex for 1 week
- Keep dressing on for 2 days, followed by daily dressing changes with bacitracin/ xeroform/ kling wrap and splint.
- Elevation of hand as much as possible
- Follow-up PRS clinic in 1 week

