Malignant (Marjolin’s) Ulcer (Verrucous Carcinoma) of Left Popliteal Fossa.
Elof Eriksson, MD
History:
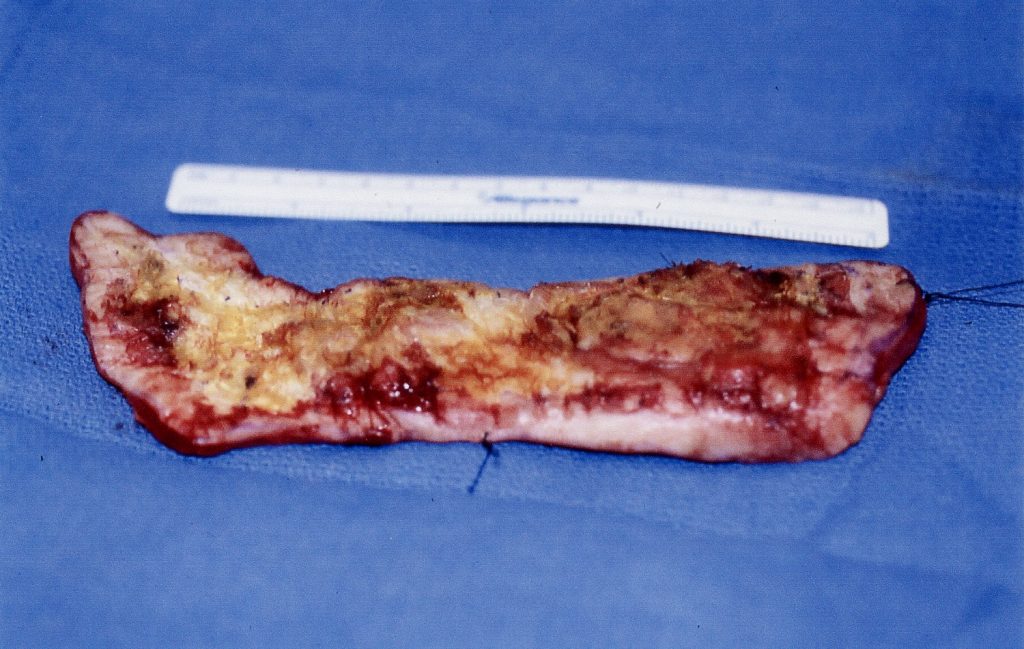
49 year old man with a history of a 95% BSA full thickness flame burn from a gas explosion 15 years earlier. The only unburned parts were his feet, his hands and the volar part of the left forearm. numerous skin grafts had been taken from his left forearm for surgical expansion and grafting. He also received Cultured Epithelial Autografts on both legs. He had had many skin breakdowns particularly on his legs. The current one over his left popliteal fossa and adjacent posterio-medial thigh and lower leg showed areas of shin breakdown and surrounding hyperkeratotic areas. These areas had initially been grafted with Cultured Epithelial Autografts. Punch biopsies were taken in order to rule out malignancy. These biopsies showed verrucous (squamous) carcinoma. A resection with a 2cm macroscopic margin was done. The resected specimen was 22 X 6cm. Permanent section section pathology showed clear margins and he was taken to the operating room two days later for grafting with expanded split thickness skin grafts under local anesthesia as an outpatient.
Findings:
49 year old man who ha severely scarred skin everywhere except on his hands and feet. In the left popliteal fossa and extending vertically up and down, there is a 22 X 6 cm area which is partially ulcerated partially keratinized. Biopsy has shown verrucous carcinoma. There are no palpable lymph nodes in the popliteal fossa or groin.

Diagnosis:
History of 95% BSA full thickness burn. Frequent skin breakdowns in left popliteal fossa. Malignant ulcer of left popliteal fossa. Biopsy showed verrucous carcinoma (Marjolin’s ulcer}
Differential Diagnoses:
Other types of squamous cell carcinoma. Basal cell carcinoma.
Workup Required:
Careful examination of popliteal fossa and groin to R/O lymphadenopathy. Chest x-ray.
Plan:
Resection with wide margins and specimen processing for permanent pathology (not frozen sections). Mesh grafting when margins are negative.
Expertise Needed:
Plastic Surgeon or Oncologic Surgeon.
Treatment:
With the patient prone and under local anesthesia with .5% Lidocaine local anesthesia, the tumor was resected with a 10 mm lateral margin and including the fascia in the deep margin. After careful hemostasis, the wound was packed with saline gauze and an elastic wrap while waiting for the pathology report. The patient was discharged on oral pain medication.
Pathology showed margins free of tumor and the wound was closed 48 hours after the resection. A split thickness skin graft, 10/1000 inch thick was taken from the left forearm, meshed , expanded and sutured in place with 4.0 chromic gut. Xeroform gauze, dry gauze and an elastic wrap was used to provide a pressure dressing.
Follow Up:
One week following skin grafting there was complete take of the graft. Three weeks later the area was fully epithelialized.

References
Massive Marjolin's ulcer in a burn graft site 46 years later
Marjolin's Ulcer Arising in a Burn Scar. Sisti A, et al. J Burn Care Res. 2018. PMID: 2959668
Current concepts in the management of Marjolin's ulcers: outcomes from a standardized treatment protocol in 16 cases
https://pubmed.ncbi.nlm.nih.gov/19349873
https://pubmed.ncbi.nlm.nih.gov/29596683
https://pubmed.ncbi.nlm.nih.gov/20662151

