Ischial Pressure Sore closed with Muscle and Skin Flap
Elof Eriksson, MD
History:
The patient is a 43 year old woman who has been paraplegic since a motorcycle accident 6 years ago. She is wheelchair bound. A right ischial pressure sore developed 3 years ago and has not healed in spite of optimal wound care and better cushions for reducing pressure on the ischial area. She is referred to plastic surgery for surgical closure of her pressure sore.
Findings:
43 year old woman in a wheel chair, who is alert and oriented and with a healthy appearance outside of a T10 paraplegia. She has no bladder control and uses a urethral catheter. She has no sensory or motor function below the T10 level. Over the right ischium there is a 2 cm opening surrounded by callused tissue. There is no evidence of invasive infection. Probing with a metal probe reveals exposed bone without periosteum and an ulcer that is 8 cm deep and surrounding the ischial tubercle.

Fig. 1. Right ischial pressure sore.
Diagnosis:
Right ischial pressure sore involving the ischial bone in a T10 paraplegic patient.
Differential Diagnoses:
R/O urethral fistula.
Workup Required:
Xray of right pelvis to assess amount of bone destruction. Cysto-urethrogram to R/O fistula. Physical examination, routine laboratory tests including protein profile and A1C.
Plan:
Hospital admission with debridement and flap closure under general anesthesia. Referral to rehab one week after surgery.
Expertise Needed:
Plastic surgeon with expertise in treating pressure sores.
Treatment:
The patient was admitted the day of surgery and the operation was done under general anesthesia (the sometimes uncontrollable spasms made local anesthesia a less attractive option). The ulcer cavity was first stained with methylene blue and then excised in a pseudotumor fashion. An osteotome was used to excise infected bone and lower the ischium by 11/2 cm. An inferiorly based rotation flap was first outlined and elevated. Then a gluteus maximus flap was then elevated and transposed in place to cover the osteotomized ischium. Finally the rotation flap was moved to cover the skin defect. Two large suction drains were used.

Fig. 2. Drawings outlining the operation with an inferiorly based rotation flap and a gluteus maximus muscle flap.
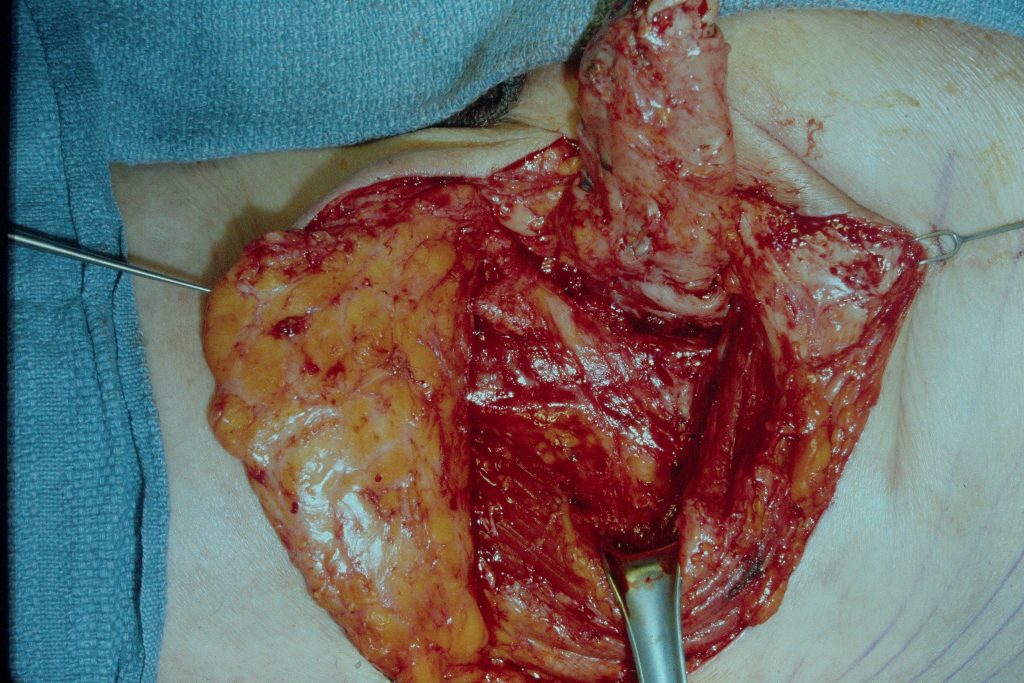
Fig.3. Both flaps elevated after resection of the pressure sore.

Fig. 4. The sutured wound.
Follow Up:
One week later, the patient was healing without any problems and was transferred to a rehab facility.
References
A dual padding method for ischial pressure sore reconstruction with an inferior gluteal artery perforator fasciocutaneous flap and a split inferior gluteus maximus muscle flap. Ku I, et al. Arch Plast Surg. 2019. PMID: 31550751 Free PMC article.
Successful reconstruction of ischial pressure sores with inferior gluteal artery descending branch perforator flap. Li H, et al. Ann Palliat Med. 2021.
Successful Pedicled Anterolateral Thigh Flap Reconstruction for a Recurrent Ischial Pressure Ulcer: A Case With Multiple Recurrences Over a 7-year Follow-up. Wang CY, et al. Wounds. 2015. PMID: 26266282
https://pubmed.ncbi.nlm.nih.gov/31550751
https://pubmed.ncbi.nlm.nih/33752419
https://pubmed.ncbi.nlm.nih/26266282

