Ischemic Foot with Threatening Infection in Patient with Diabetes and Peripheral Arterial Disease
History:
A 52-year-old male with a history of uncontrolled diabetes, dyslipidemia, and hypertension presented to the emergency department with a malodorous left foot wound. Patient related onset of wound has been three months, but the discoloration and pain began three days ago. He has not been seen by a primary care physician in over a year. Denies taking any measures, including medication, to manage his diabetes. Patient understands that he has been neglecting his health but would like every possible measure taken to salvage his affected limb.
Findings:
Upon examination the patient had non-palpable pedal pulses, forefoot crepitus, superficial skin necrosis, malodorous, purulent draining wound, and a loss of protective sensation. Diagnostic imaging, vitals, and labs confirmed septic necrotizing fasciitis infection. Furthermore, an arterial duplex ultrasound exhibited significant tibial arterial stenosis.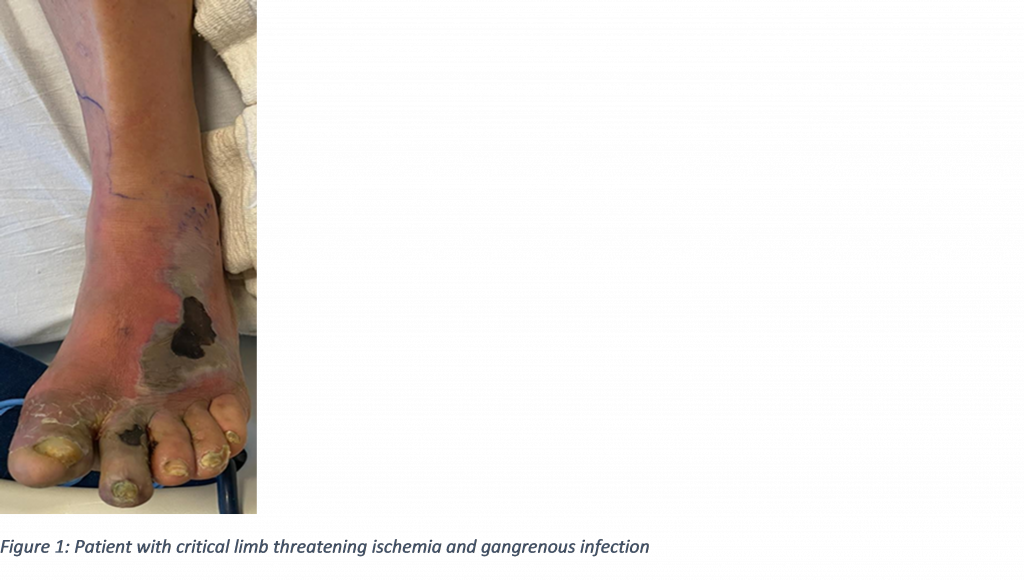
Diagnosis:
Septic Necrotizing Fasciitis complicated by Peripheral Artery Disease.
Differential Diagnoses:
Wet gangrene
Osteomyelitis
Workup Required:
X-ray imaging displayed soft tissue emphysema and osteomyelitis of hallux.
Bedside cultures taken for antibiotic adjustments.
Thorough review of medical history and NPO status as this case requires urgent surgical intervention.
Plan:
Immediate surgical irrigation and debridement of non-viable bone and tissue for infection source control. Post operative care admission as patient will require inter-service consults and close management of infection.
Expertise Needed:
Patient will require aggressive intervention by Podiatric Surgery as this is a limb threatening infection requiring staged surgeries. He will also require Vascular Surgery to address his peripheral artery disease and Endocrinology for long term diabetes management.
Treatment:
Despite lack of pedal pulses, patient received an immediate partial first ray amputation with midfoot debridement of nonviable tissue. Without prompt open amputation the patient would have remained septic in limb and life-threatening context. During admission patient received an angiogram with angioplasty of tibial vessels to provided patent blood inflow to foot. Antibiotic regimen was selected based off intra-operative cultures. Endocrinology was brought on board for glycemic control and long-term insulin management. With blood sugar control and improved vascular inflow, the patient was brought back into the operating room for a transmetatarsal amputation with application of a collagen-based graft product to expedite healing.

Follow Up:
Within two weeks of hospital discharge, patient was seen in clinic displaying no signs of infection and healthy perfusion at amputation site. At four weeks post operation the wound bed was completely granular, superficial, and reduced in size by over fifty percent. The patient completely epithelialized within three months.

