Infected venous leg ulcer
History:
A 81-year-old woman, with history of hypertension, was referred to our hospital from her primary care physician. She developed a small wound on her left lower leg after scratching two weeks ago. After that, the wound became larger and deeper, and she couldn’t walk because of severe pain.
Findings:
There was a wound 8 X 9 cm on the lateral side of her left lower leg, covered with slough and necrotic tissue. The lower half of her left leg was swollen and hot. The appearance of her lower led looked like a reverse champagne bottle shape. The skin surrounding the wound was pigmented and red. Left dorsal pedis and posterior tibial artery were palpable, and her sensation of the leg and foot was normal.
Diagnosis:
Infected venous leg ulcer of left lower leg.
Differential Diagnoses:
Ischemic foot ulcer, pressure ulcer, vasculitis, skin cancer, pyoderma gangrenosum
Workup Required:
- Ultrasound of arteries and veins
- ABI
- Laboratory test including inflammatory markers
- Culture from the deep area of the ulcer
Plan:
- Hospitalization
- Infection control by antibiotics
- Wound bed preparation including debridement
- Wound dressing
- Compression with elastic bandage
- Skin graft after completion of wound bed preparation
Expertise Needed:
Wound specialist, Wound nurse, Vascular surgeon, Ultrasound technician
Treatment:
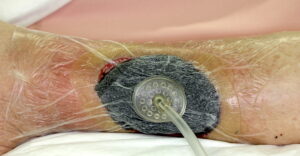
After hospitalization, culture from the deep area of the ulcer was taken and antibiotics treatment was started. Antibiotics was performed empirically fist and changed to the most appropriate based on the culture results. ABI was normal, deep venous thrombosis was excluded by ultrasound and there was no indication for varix surgery. We ordered her bed rest and applied an elastic bandage on her lower leg. Her wound was washed and covered with moist wound dressing every day. 5 days later, sharp debridement was performed under general anesthesia. Necrotic and infectious tissue including fascia was fully debrided, and negative pressure wound therapy (3M™ ActiV.A.C.™ Therapy System; 3M) was applied. After three weeks, her wound was covered with good granulation tissue, and a mesh skin graft was performed in the operating room. Her wound healed completely.


Follow Up:
After six years, she could walk with compression stocking and there was no recurrence.

