Degloved Plantar Wound
Findings:
.

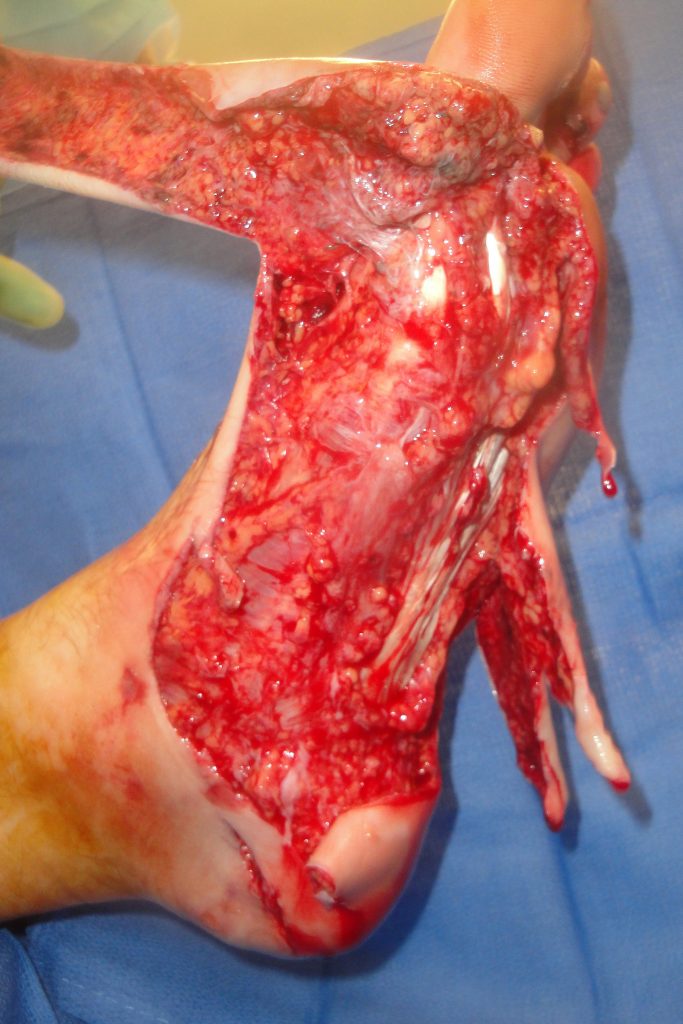

Fig.1. Complex plantar degloving lacerations of the left foot on the day of injury.
The plantar wounds involved a majority of the left foot plantar surface as shown
Diagnosis:
Differential Diagnoses:
Workup Required:
Plan:
Expertise Needed:
Treatment:
Initial wound cleaning and debridement was accomplished with syringe and then judicious hydrosurgical dissection and debridement (Figure 1). Minimal trimming of the distal ends of the flaps was done initially to let viability.be determined at a later date after full circulatory resuscitation and treatment with an Extracellular Matrix wound devices and negative pressure wound therapy had been attempted.
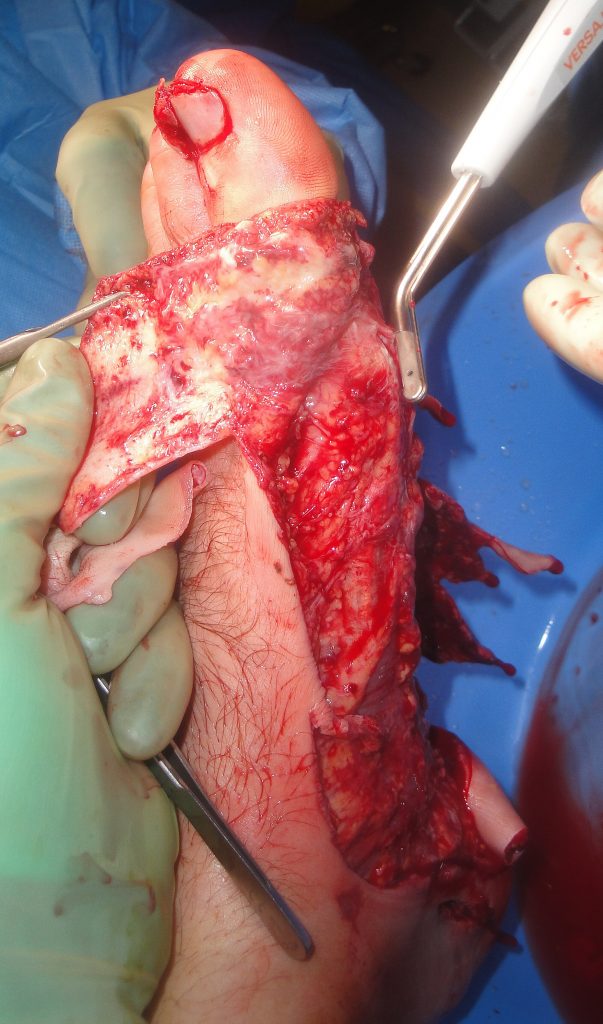
Fig.1. UBM treatment

Fig.2. Further UBM treatment

Fig.3. Full plantar aspect after UBM treatment

Fig.4. Negative pressure dressing over UBM.
Follow Up:
Negative pressure wound therapy was used for the first 3 weeks and then again for 1 week after split thickness skin grafting done at post-operative week 4. During this time the NPWT dressing was changed weekly and the outer wound slough and desquamated skin was rinsed off before replacing a new vaseline impregnated gauze and piece of black foam. Moisture retentive dressings were used until there was wound closure. This consisted of either a polyurethane sheet dressing or hydrogel with a non-adherent dressing. He was able to ambulate small distances beginning at 3 months and was fully ambulatory with a padded sole shoe at 4 weeks. He regained complete sensation of his plantar surface and was able to ambulate on 4-5 hour hikes and felt no serious limitations. He had normal tissues over the main pressure points of his plantar surface and the healed incision lines had soft supple scars.
Clinical Note– Over time there was replacement of the skin grafted wound with normal plantar tissues which was not scar retraction of the skin grafts which can be seen in the clinical photos.

Fig.5. Post-OP healing week 2


Fig.6. Wound healing at week 4 at the time of plantar split thickness skin grafting

Fig.7. Plantar healing 2 weeks after split thickness skin grafting


Fig. 8. Final plantar wound appearance 14 months post-injury

