Closure of a large tissue defect after hallux valgus operation
History:
A 26-year-old female patient without previous diseases had a hallux valgus operation in an orthopedic clinic. During the first operation the orthopedic surgeon was not able to close the wounds and a soft tissue defect remained. Therefore, the patient received VAC-therapy. Multiple VAC-therapy cycles were performed. As the wound could not be closed after 10 weeks, the osteosynthesis was removed. However, a soft tissue defect on the arch of her left foot remained and the patient received another VAC-therapy. Afterwards the patient was presented to our department of plastic and reconstructive surgery.
Findings:
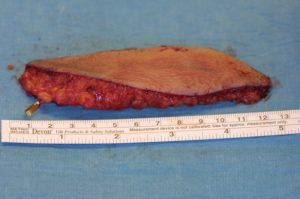
During the intraoperative examination in the department of plastic and reconstructive surgery, we measured a soft tissue defect of about 8 x 4 cm on the arch of the left foot. The musculus flexor hallucis longus tendon and the first metatarsal bone were exposed.

The caput of os metatarsale I was nonviable and therefore needed to be removed.
Diagnosis:
Postoperative soft tissue defect at the left foot with exposed tendons and bone.
Differential Diagnoses:
Wound infection
Workup Required:
Doppler-sonography at the donor-site of the free flap, blood-examination, blood-grouping, diagnostic imaging of the foot
Plan:
For the treatment plan, not only a sufficient soft tissue reconstruction to cover the bone and tendons but also the functional outcome was taken into account. The soft tissue reconstruction should allow the patient to wear normal shoes, without the need of an orthopedic shoe provision. This is to ensure that the young patient can live a normal life without stigmatization and can continue to play sports. Considering the age of the patient, the aesthetic purpose was also taken into consideration. As the tissue defect was too large for a regional tissue reconstruction, we recommended a free flap. The patient refused to get an ALT-free flap or a Musculus latissimus dorsi-free flap, as she was concerned that it might wear out. The patient preferred a parascapular- or a lateral upper arm-free flap. We explained that there might be large scars at the donor-site. The patient agreed to that.
Expertise Needed:
Plastic surgeon with expertise in microsurgery and free flap procedures
Treatment:
The patient had multiple VAC-therapy cycles for wound conditioning.

After the debridement, the entire soft tissue defect of the foot with exposed tendons and bone were visible.

The caput of os metatarsale I was nonviable and therefore needed to be removed.

The plastic surgeon decided to perform a lateral upper arm- free flap. Firstly, the vessels at the recipient-site were prepared. Arteria dorsalis pedis and two accompanying veins were identified. Subsequently, the lateral upper arm- free flap was dissected.

Using an operating microscope, the free flap was anastomosed end-to-end to the Arteria dorsalis pedis. Furthermore, two veins were anastomosed to ensure a sufficient venous backflow. Drains were placed and subcutaneous and skin sutures were performed.

Follow Up:
The patient was observed at the intensive care unit for one night after surgery. The free-flap was monitored hourly in the first 24 hours by a clinical examination and doppler ultrasonography. For the next 24 hours, the free flap was monitored every two hours and the next day every four hours. The drains were removed after a few days. The sutures were all removed in post-operative week 3. The patient had physiotherapy. The patient had to take Aspirin for 10 days and got a thrombosis prophylaxis and a sufficient pain medication. After patient discharge the patient had control examinations in our clinic. The wound healing was without complications. The patient was satisfied as she had normal gait in normal shoes and was not compromised in her daily activities.



