Large Shoulder Wound
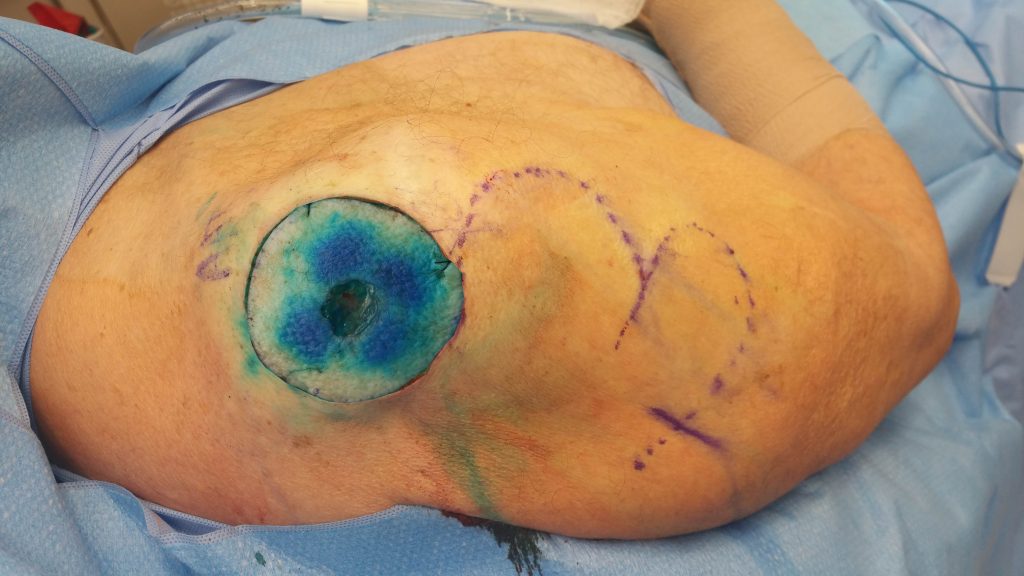
Fig. 1. Pre-operative photo (compilation) of a large apex shoulder surgical defect
Findings:
Full-thickness circular surgical defect of 65 mm diameter on the apex of the right shoulder immediately following wide local excision. There was significant laxity of the surrounding tissues and several healed scars anteriorly on the shoulder.

Fig. 2. The excised skin

Fig. 3.The resultant defect with the outline of a bi-lobed flap.
Diagnosis:
Acute, full-thickness surgical wound after wide local excision in a 76-year-old patient with previous rotator cuff surgery and complex cardiac history.
Differential Diagnoses:
None required
Workup Required:
Only routine physical examination and laboratory tests.
Plan:
- No additional workup was required
- Immediate reconstruction following wide local excision
- Closure with a local random-pattern skin flap, which would favor the anatomy and account for skin laxity and previous scars from surgery
- Support the wound closures with Dermabond and Steri-Strips
- Follow up on POD 10, 24, 31
Expertise Needed:
Plastic Surgeon
A surgeon with experience with local flaps
Treatment:
Initially, primary closure was planned; however, significant tension, previous scars, and potential limitation in mobility led to an adjustment of closure options1.
Local flap coverage2 was favored, and a bilobed local skin and subcutaneous tissue transpositional flap closure was performed3–6. The flap axis was directed inferior and lateral to the resection site, with the first lobe measuring approximately 6.5 cm and the second lobe measuring approximately 4 cm. The skin was anesthetized utilizing local anesthetic (Lidocaine 1%), and an incision was created in the bilobed flap. This was carried down through the subcutaneous tissue to the muscular fascia of the right upper arm. The flap was then elevated off of the muscular tissue for the entirety of the flap, which measured approximately 10 x 10 cm. Once elevated off of the muscular fascia, this was able to be rotated up with the first lobe placed into iatrogenic defect of the right shoulder. The second lobe replaced the first lobe and the inferior aspect was brought together primarily. The wound was copiously irrigated with normal saline until the effluent was clear and meticulous hemostasis was ensured. The wound was then brought together utilizing buried, interrupted 3-0 Vicryl deep dermal sutures approximately every 0.5 cm along the entirety of the wound. The skin itself was brought together utilizing running 4-0 Monocryl subcuticular sutures. The right upper arm was then washed and dried and half-inch Steri-Strips were applied to all incision sites followed by Dermabond as a protective layer.

Fig. 4. Testing flap reach to close the defect.

Fig. 5. Immediate postoperative view
Follow Up:
By 3 weeks, the incision was completely healed.

Fig. 6. Three weeks after surgery the flap was well perfused and healing well.

