Chin laceration
History:
A 26 year old male with left chin laceration sustained during a motor vehicle accident. He denied any loss of consciousness or any other injuries. He reported moderate bleeding from his left chin that was controlled with pressure. TDAP was given in the ED. No further imaging or labs were obtained by the emergency department. The Plastic and Reconstructive Surgery team was consulted for the chin laceration.
Findings:
On exam, 4 cm long, deep laceration to the left chin, with exposed mentalis muscle. The laceration was deep but with no intraoral component. There was no loss of teeth or evidence of facial fractures.


Figure 1-2. Show left chin laceration.
Diagnosis:
Complex laceration of left chin.
Differential Diagnoses:
Chin laceration, r/o injury to mental nerve.
Workup Required:
Cranial Nerves 2-11 were tested and were without deficit although there were mildly decreased sensation to the left chin compared to the right. The laceration was inferior to the mental foramen and the mental nerve was intact. No intraoral lacerations, malocclusion, or loose teeth were noted on exam. Consent was then obtained for irrigation, debridement, and closure of his chin laceration.
Plan:
Repair of the laceration under local anesthesia in the Emergency Department.
Expertise Needed:
Plastic surgeon.
Treatment:


Figure 3-4. Show repaired left chin laceration.
Follow Up:
One week for removal of non-resorbable sutures, followed by 1 month follow up for healing. Additional follow ups as needed depending on scar maturation and healing.
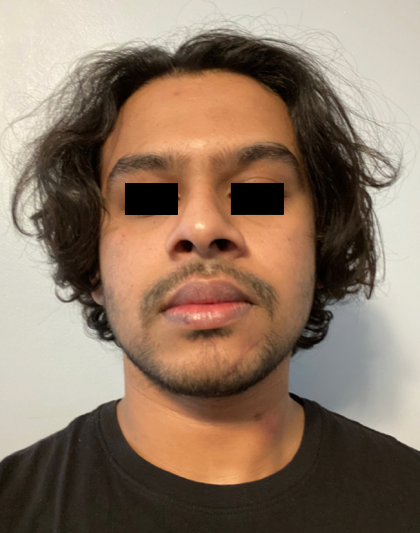
Figure 4. One month follow up.

