Upper Back Wound from Chondrosarcoma Resection
History:
Findings:
40 year old male with a 8x10cm superior left back mass, nonmobile, no overlying skin changes aside from healing biopsy site. Bilateral latissimus dorsi muscles present bilaterally.
Diagnosis:
Differential Diagnoses:
Workup Required:
CT chest, abdomen and pelvis was negative for metastatic disease. MRI showed a large 12.5×6.1×7.8 cm mass with involvement of spinous process and lamina of T1 and T2. Surgical oncology and neurosurgery consulted who recommended radical resection of the posterior trunk tumor, laminectomy with posterior spinal fixation in conjunction with plastic surgery reconstruction.
Plan:
Resection of the spinal/paraspinal tumor (Sarcoma), laminectomy and posterior fixation of thoracic spine (Neurosurgery), with musculo-cutaneous flap reconstruction (Plastic Surgery).
Expertise Needed:
Treatment:
Plastic surgery then proceeded with reconstruction of complex left posterior trunk defect with a compound extended latissimus dorsi myocutaneous flap based on the left thoracodorsal vessels and transverse scapular flap based on circumflex scapular vessels (22x33cm) to achieve adequate soft tissue coverage. The flap design was as a very large “V” skin incision embracing the lower aspect of the defect and extending beyond the midline. The upper part of the flap was raised deep to the fascia to include the transverse branches of the circumflex scapular vessels at the base of the flap. The anterior and posterior borders of the latissimus dorsi were identified and the flap elevated from inferior to superior off the underlying serratus anterior. When fully mobilized, the flap was able to rotate and advance into the defect.
Additionally, due to the irregular contours created by the hardware and in order to eliminate any areas of dead space, local muscle would be required to help cover the exposed hardware. The distal part of the left trapezius muscle was elevated based on perforators from the intercostals. This was turned over to cover the majority of the hardware. The local left-sided rhomboid muscle flap was elevated and advanced to cover the remaining hardware. The myocutaneous flap was then advanced into the defect in a V-Y fashion and three drains were placed. This was closed in a layered fashion with interrupted 3-0 Vicryl deep dermal, 3-0 V-Loc intracuticular and running 3-0 Prolene for skin. The flap appeared well perfused at the end of the case.

A. Preoperative mass with healed biopsy scar

B. Intraoperative defect (15x15cm) and markings for compound extended left latissimus dorsi myocutaneous flap and transverse scapular flap. Marked landmarks include scapula, latissimus dorsi muscle, posterior midline and extended skin paddle
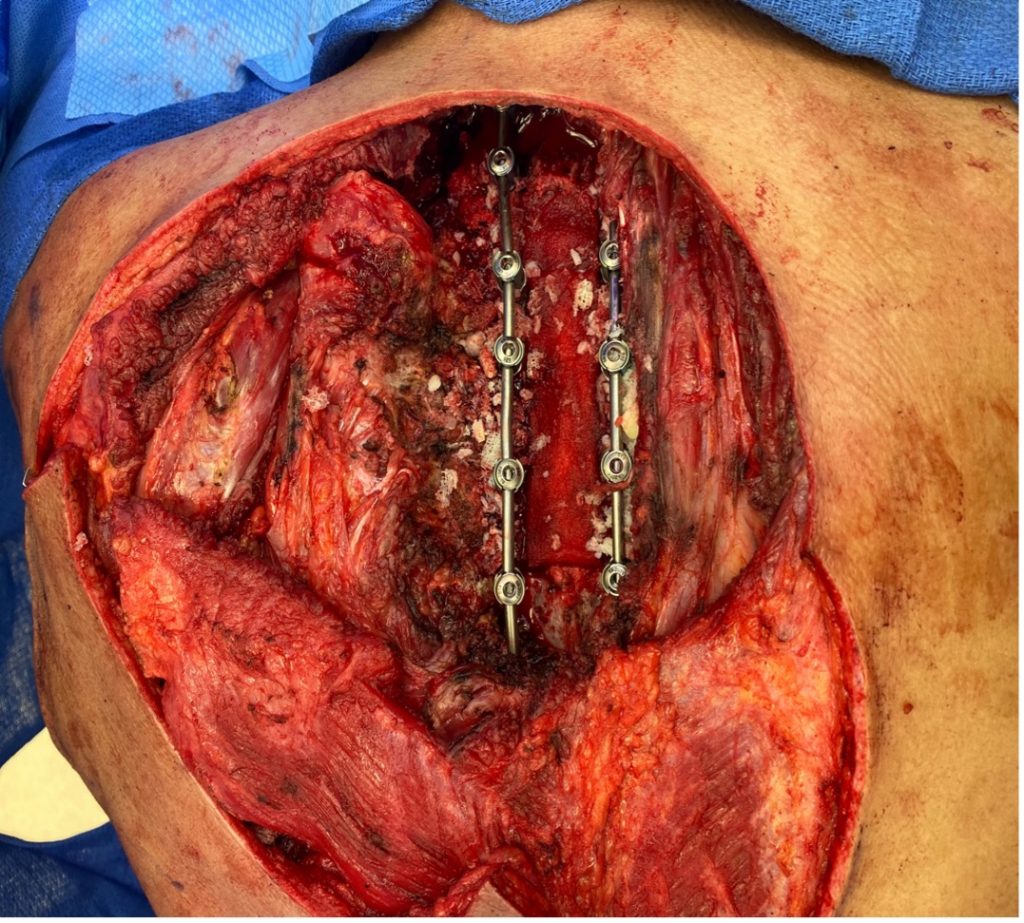
C. Posterior trunk defect with exposed hardware
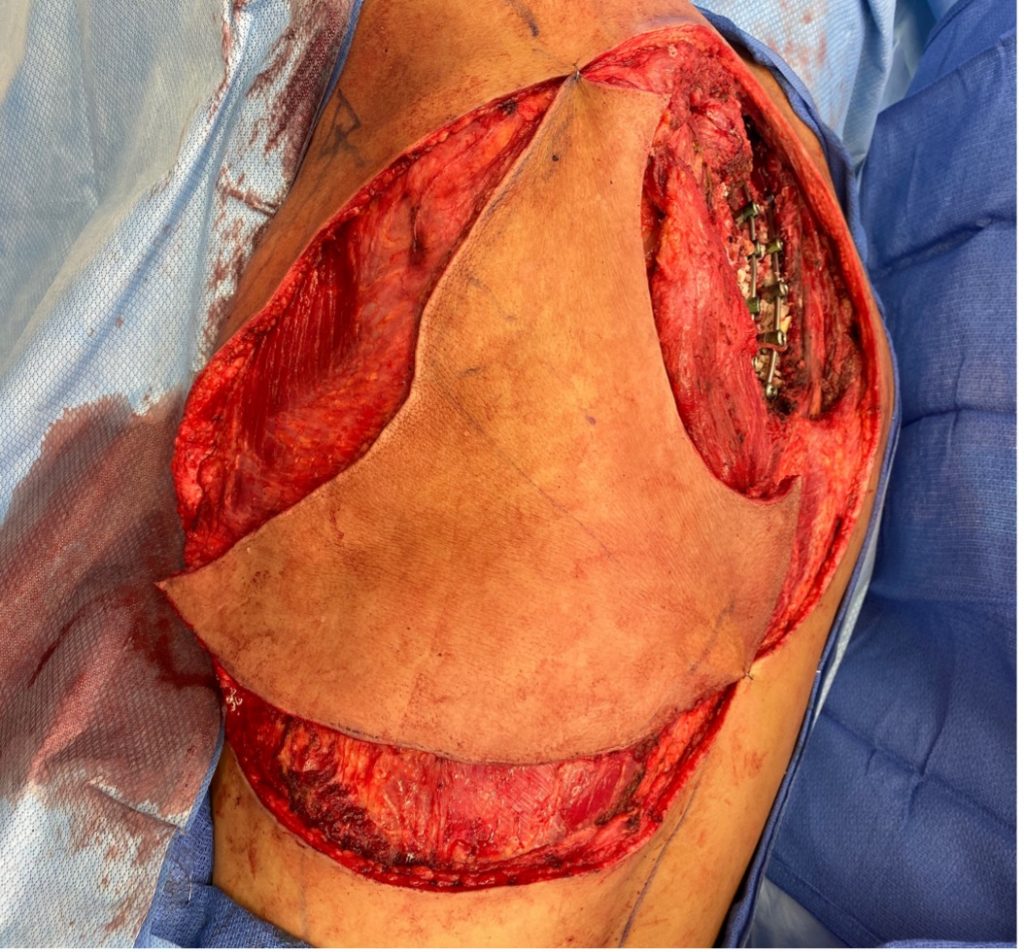
D. Compound extended left latissimus dorsi musculo-cutaneous flap and transverse scapular flap, elevated
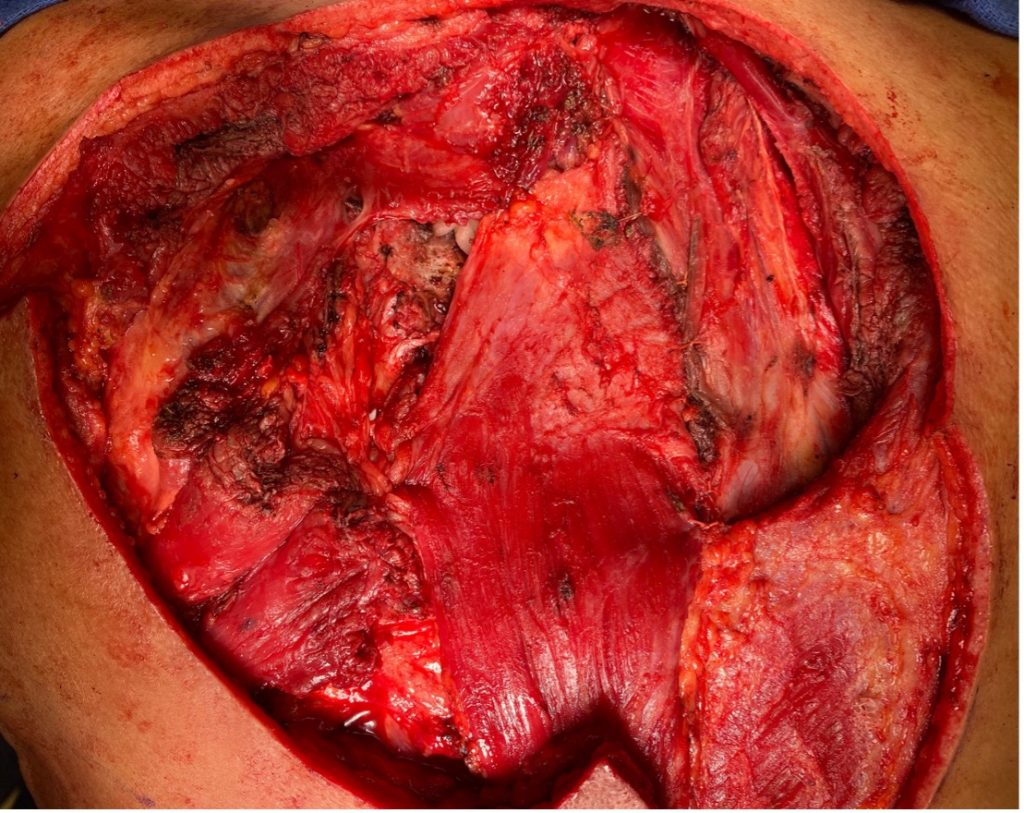
E. Coverage of hardware with local turnover of left lower trapezius muscle flap and local left rhomboid muscle

F. Post operative advancement and inset of flap

G. Flap healed at 2 month follow up without necrosis, dehiscence or infection
Follow Up:
Final surgical pathology showed focal involvement of the deep margin necessitating adjuvant radiation. Sutures and all drains were all removed by post operative week 3. Unfortunately he developed a recurrence in the left paraspinal region involving T3-T extending to the neuroforamen and underwent re-resection of the T3-T5 paraspinal/epidural tumor with removal of hardware and did not require any additional reconstruction at this time. He is planned to complete another round of adjuvant radiation with close monitoring.

