Elbow wound closed with two opposing rotational flaps (Ying-Yang).
History:
A 47-year-old woman with a past medical history significant for ataxia due to traumatic brain injury, repeated falls, and fractures. As a result of a fall, she developed right olecranon bursitis and underwent a bursectomy with fistulectomy by an orthopedic surgeon that was complicated with wound dehiscence (Figure 1). Subsequent management consisted of antibiotics, routine dressing changes, and splinting; however, after three weeks, the wound was not healed, and the patient was referred to plastic surgery service for evaluation.

Figure 1. Elbow wound resulted after dehiscence post bursectomy and fistulectomy
Findings:
Diagnosis:
Differential Diagnoses:
Chronic infection
Incomplete bursectomy and fistulectomy
R/O osteomyelitis
Other issues: tissue tension, smoking, diabetes, malnutrition/hypoalbuminemia, advanced age, previous scar or cancer at the site of the wound1.
Workup Required:
CBC, inflammatory markers (CRP, ESR), Albumin/Prealbumin, blood glucose, HgA1C
Plan:
- Outpatient workup to discuss the options with the patient.
- Surgical exploration, debridement of devitalized tissue, and no tension closure.
- Wound culture.
- Antibiotic therapy for surgical prophylaxis.
- Two opposing rotational (Ying-Yang) fascio-cutaneous flaps to close a dehisced wound on the elbow.
- Period of immobilization/limiting activity after surgery to prevent rupture.
- Follow up weekly for four weeks, and one last follow-up a year from post-op.
Expertise Needed:
Plastic Surgeon
Treatment:
The patient was placed under general anesthesia, prepped, and draped sterilely. The nonhealing right elbow wound was sharply debrided, and intraoperative cultures were obtained. Necrotic tissue and bursa were excised entirely, and a pulse lavage was performed (Figure 2). The resultant defect measured 3 x 5 cm. The wound could not be closed primarily. Therefore, two opposing rotation fasciocutaneous flaps were created. The flaps were then progressively dissected-rotated until no tension closure was achieved (Figure 3). Tension was also tested with elbow flexion. Exparel, a local infiltrative anesthetic, was used for postoperative pain control. The elbow was noted to move freely when flexed and extended (Figures 4 & 5). Subsequently, the closure was performed with single interrupted deep dermal Monocryl 4-0 sutures and 3-0 Nylon in a vertical mattress fashion. The incisions were dressed with Xeroform, followed by dry sterile fluff dressing and loosely wrapped ACE wrap4. The patient tolerated the procedure well and was admitted to the recovery room in stable condition. The patient has been prescribed 100 mg of doxycycline twice daily for one week and 250 mg of erythromycin every six hours.
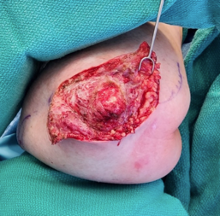
Figure 2. The right elbow wound was opened, evaluated, and aggressively debrided

Figure 3. Intraoperative photo of the fascio-cutaneous flaps dissection and progressive approximation to eliminate closure under tension.

Figure 4. Intraoperative photo of the elbow wound closure with Ying-Yang fascio-cutaneous flaps with the elbow flexed with no tension on the incision

Figure 5. Intraoperative picture of the elbow wound closure with Ying-Yang fasciocutaneous flap with the elbow in extension with no tension on the incision
Follow Up:
Cases with repeated wound dehiscence should be monitored closely due to the potential for infection or dehiscence. Findings from previous wound cultures before surgery grew a rare Enterococcus faecalis infection sensitive to doxycycline. One-week post-op, the patient was healing as expected and reported minimal serous discharge (Figure 6). After the second-week patient presented to the emergency department with concerns of increased drainage and erythema to the surgical incision, which grew Staphylococcus epidermidis and a rare Enterococcus faecalis on cultures. The patient was seen by the plastic surgery service and was started on linezolid (Figure 7). Three weeks post-op, the cultures were taken, and no bacteria grew (Figures 8 & 9). On week four post-op, the patient was advised to add Medihoney to the cleaning routine to ensure wound healing, and sutures were removed. The patient was followed up via telehealth call after six weeks which showed the wound was healing well. The last one-year follow-up showed complete closure and healing of the wound (Figure 10).

Figure 6. One-week postoperative photo of the elbow wound closure with fasciocutaneous flaps, elbow in flexion

Figure 7. Postoperative photo two weeks after Ying-Yang flap closure with erythema and increased drainage.

Figure 8. Postoperative week three from closure, elbow in flexion.

Figure 9. Postoperative week three from closure, elbow in extension

Figure 10. One year follow-up showed complete closure and healing of the wound.

