Ischemic fingertip partial avulsion injury
History:
A 42-year-old right hand dominant female with a history of alcoholism, hypertension and hypothyroidism presents after she accidentally stuck her left hand in a hedge trimmer 4 hours prior. Patient was attempting to clean the trimmer when it was unexpectedly activated. Patient states she has had a prior left endoscopic carpal tunnel release several years ago. She denies any other injuries. She comes to the ED for evaluation. Patient is an active smoker with a 20-year pack history.
Findings:
On exam: Left ring finger with distal oblique partial amputation extending to the DIPJ with no exposed bone. Injury extends proximally 3 cm towards the DIPJ. Avulsed tissue appears dusky with significant venous congestion, poor capillary refill, with diminished sensation to light to touch. flexor tendons and extensor mechanism intact.
X-ray shows a displaced distal tuft fracture

Figure 1. Injured pulp with deep involvement

Figure 2. Injured pulp with deep involvement and duskiness

Figure 3. Ischemic discoloration of the pulp tip
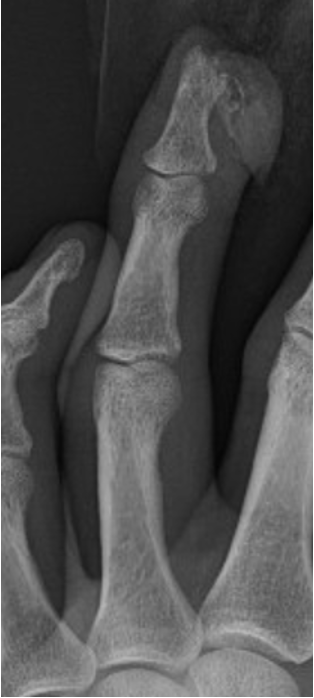
Figure 4. Oblique XR of the digit with distal phalanx fracture

Figure 5. AP XR of the digit with distal phalanx fracture

Figure 6. Lateral XR of the digit with distal phalanx fracture
Diagnosis:
Left ring finger tip near complete amputation with ischemia.
Differential Diagnoses:
Workup Required:
Imaging including X-ray, prior vaccinations including last tetanus. Routine laboratory studies.
Plan:
In ED, washout, defatting of the avulsed fingertip and repair as a composite graft
Expertise Needed:
Plastic or Hand surgeon.
Treatment:
5cc of 1% lidocaine without epinephrine was injected at the volar base of digit and across the dorsum for a digital nerve block. A tourniquet was then placed using a Penrose drain and Kelly clamp . Irrigation using approximately 1 L of dilute betadine was completed ensuring no visible bone or tendon. The avulsed tip was then defatted to the deep dermal layer using a curved iris scissors, similar to defatting a full thickness skin graft. After adequate hemostasis, the avulsed tip was approximated to the pulp using 4-0 chromic in an interrupted manner. The composite graft was then fenestrated with two 5mm incision using an 11 blade to allow drainage. Given intact nail fold and no underlying injury to the remaining nail bed, there was no need for nail plate removal. An aluminum foam splint was placed over the distal and middle phalanx and the patient was informed that dressing should be replaced at follow up in 1 week. Patient was told to stop smoking and referred to a cessation program given increased risk for infection. Patient was prescribed one week of Keflex and was to follow up in one week and to call back sooner if he developed any signs of infection.

Figure 7. Digit after immediate repair
Follow Up:
The patient followed up in 1 week and the fingertip was found to be slightly ischemic with diminished sensation. Patient instructed to continue local wound care with bacitracin and xeroform, and again instructed to quit smoking.

Figure 9. 2 month follow up with marked improved in scar formation and improved perfusion

