Ischial pressure sore
Dmytro Unukovych, MD PhD
, Alexander Larsson, MD
History:
A 47-year-old woman with a history of a recent spinal cord injury presented with a non-healing ischial pressure sore. Despite previous attempts at conservative management with offloading, intensive wound care, including revisions and NPWT, the wound persisted.
Findings:
The patient, who was paraplegic but otherwise healthy, was a non-smoker with a normal BMI. A grade IV pressure sore measuring 4x4x5 cm was present over the left tuber ischii, involving the bone, yet without significant undermining of the skin. The sore walls were fibrotic and had formed a chronic thick capsule. There were no signs of active infection observed either on the skin or in the wound status, and microbial swabs identified skin flora.

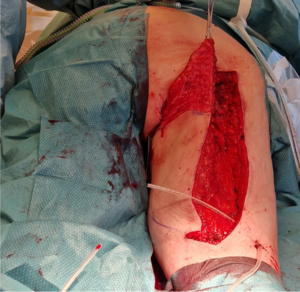
The ischial pressure sore stained with methylene blue to facilitate complete removal. A posterior thigh advancement flap has been outlined.
Diagnosis:
Grade IV pressure ulcer in paraplegic patient
Differential Diagnoses:
R/O extensive undermining and urethral injury.
Workup Required:
Wound microbial swabs, blood tests (albumin, hemoglobin)
Plan:
Hospital admission one day preoperatively, surgery extent: wide local excision of the wound with flap reconstruction, 2 hours under general anesthesia
Expertise Needed:
Plastic surgeon with experience of local flaps in the region
Treatment:
Under general anesthesia, the interior of the pressure sore was stained with methylene blue and then excised en bloc, leaving approximately a 2 cm margin between the wound wall and healthy, well-vascularized tissues. The exposed cortex of the tuber ischii at the base of the wound was removed using an osteotome (approximately 4 mm). Both the wound specimen and the bone were sent for microbiological assessment.

The resulting defect was larger than the skin opening and required additional padding (Figure 2). A random posterior thigh flap was incised according to pre-markings, initially to the level of the fascia. The muscle fascias were then meticulously released all around the flap, allowing for easy cranio-medial sliding. The flap reached the defect without the need for flap undermining or muscle division. The skin of the flap was deepithelialized to provide padding for the wound (Figure 3).
Parachute Vicryl 0 sutures were used to secure the padding to the periosteum/ligaments over the tuber ischii. Subsequently, the flap was sutured with Vicryl 2/0 at the level of the Scarpa’s fascia, subdermally, and finally with Ethilon 3/0 on the skin. The vertical incision was closed intradermally with Stratafix 3/0 sutures. Two active drains were inserted: towards the wound bed and under the distal part of the flap.

Follow Up:
After the procedure, the patient remained in a supine position on an air-fluidized therapy bed for 7 days. Offloading continued during the subsequent two weeks at the rehabilitation center, under the supervision of a dedicated team of physiotherapists who monitored the flap throughout all stages of patient mobilization.
Drains were removed on POD 4 and the sutures on POD 21.
The recovery was uneventful with confirmation of satisfactory result one year postoperatively.
References
Djedovic G, Morandi EM, Metzler J, Wirthmann A, Matiasek J, Bauer T, Rieger UM. The posterior thigh flap for defect coverage of ischial pressure sores - a critical single-centre analysis. Int Wound J. 2017 Dec;14(6):1154-1159. doi: 10.1111/iwj.12776. Epub 2017 Jun 29. PMID: 28661069; PMCID: PMC7950091.
Bialowas, Christie M.D.; Nguyen, Brittany M.D.; Patel, Ashit M.B.Ch.B.. Best Solutions for Perineal and Pressure Sore Reconstruction. Plastic and Reconstructive Surgery 148(6):p 1026e-1039e, December 2021. | DOI: 10.1097/PRS.0000000000008509
Vathulya, Madhubari MS, MCh (Plastic Surgery)a; Praveen, A.J. MS (ENT), MCha; Barik, Sitanshu DNB (Orthopedics)b; Jagtap, Manish Pradip MS (GENERAL SURGERY) MCha; Kandwal, Pankaj MS (Orthopedics)b. A Systematic Review Comparing Outcomes of Local Flap Options for Reconstruction of Pressure Sores. Annals of Plastic Surgery 88(1):p 105-113, January 2022. | DOI: 10.1097/SAP.0000000000002941
https://onlinelibrary.wiley.com/doi/10.1111/iwj.12776
https://journals.lww.com/plasreconsurg/fulltext/2021/12000/best_solutions_for_perineal_and_pressure_sore.42.aspx?casa_token=_O3ZG7NtilIAAAAA:8l17YpZkEa-mDYQ5er58UQvL0v6EYqUy_6GIHHHDx5lrfkWUFu0SzN9G6DchJ_AEPaa_QL81heSoc-TM2Xpl8XxoJg
https://journals.lww.com/annalsplasticsurgery/fulltext/2022/01000/A_Systematic_Review_Comparing_Outcomes_of_Local.21.aspx?casa_token=xZUtyvBS5_0AAAAA:bPwda3eRnNvZ2ZXwREdHmNvXCLFxWrIE6hmSGUEI5QOJhtulKh9YzvnKccvlYOadQkdsXAkp45vt88HC0--WPPF_UA

